HOSSEIN SADEGHI-NEJAD, ANOOP SHARMA, ROBERT J. IRWIN, STEVEN K. WILSON, AND JOHN R. DELK
ABSTRACT
Objectives. To obtain data concerning the incidence and management of reservoir herniation in inflatable penile prosthesis surgery in a clinical investigation. Reservoir herniation after scrotal placement of inflatable penile prosthesis is an unusual complication, and a review of the published medical reports reveals only anecdotal reports and no definitive articles.
Methods. A multi-item self-addressed questionnaire was mailed to the members of the Society for the Study of Impotence questioning the occurrence of reservoir migration from the prevesical space to the inguinal canal or scrotum. In addition, the database of one of us was reviewed to determine the incidence of reservoir migration in a large series of 1206 three-piece penile prostheses.
Results. The response rate was 38%. A minority of respondents (28%) were familiar with the problem. Of those who had experienced this complication, the occurrence was very rare and usually appeared in the immediate postoperative period, often in association with vigorous coughing spells or vomiting. The responders also indicated that imperfect surgical technique might have been implicated in some cases. Management usually consisted of reservoir replacement or repositioning through an inguinal incision with repair of the defect. Alternatively, several surgeons used the existing scrotal incision if the patient presented in the immediate postoperative period. The incidence of reservoir herniation was 0.7%.
Conclusions. Reservoir herniation is a rare complication of inflatable penile prosthesis surgery that occurs almost exclusively in penoscrotally placed prostheses. Familiarity with various approaches to the management of this complication is clinically useful to urologists performing penile prosthesis surgery. UROLOGY 57: 142–145, 2001. © 2001, Elsevier Science Inc
Inflatable three-piece prostheses have become remarkably mechanically dependable. Although earlier models were notable for high mechanical failure and leakage rates, recent reports have demonstrated overall 5-year revision-free survival rates as high as 93%.1,2 Most device revisions are for human factors (infection, medical problems, physician error in technique, or patient dissatisfaction) rather than mechanical malfunction. Although the volume of published reports concerning various medical complications is large, very little could be found regarding the complication of reservoir herniation after scrotal implantation of three-piece prostheses. A review of recent medical-surgical text chapters on penile prosthesis surgery and complications also yielded no information on this topic, although a few reports were noted on small and large bowel erosions of prosthesis reservoirs. 3–5 This questionnaire study was designed to address some of the issues concerning the diagnosis and management of inguinal/intrascrotal reservoir herniation. In addition, the database from the records of one of us (S.K.W.) was reviewed to determine the incidence of reservoir herniation in a large series.
MATERIAL AND METHODS
A multi-item questionnaire was mailed to 275 members of the Society for the Study of Impotence (SSI). The questionnaire addressed the demographic data and percentage of practice devoted to erectile dysfunction, the number of prostheses placed per year, the type (semirigid versus multicomponent inflatable) and brand of prostheses used, the approach (infrapubic versus penoscrotal), the location of reservoir placement, and the physician’s experience with reservoir herniation. Physicians who had experienced reservoir migration were asked to comment on the site and timing of the herniation and on their preferred operative approach for the correction of this complication.
The database from the records of one of us (S.K.W.) was reviewed to determine the incidence of reservoir herniation in a large series of 1206 inflatable three-piece penile prostheses placed from 1991 to 1997.
RESULTS
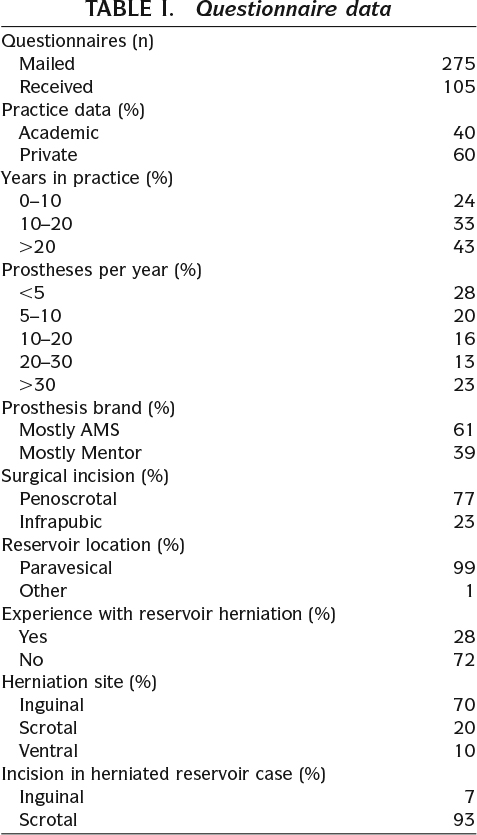
One hundred five questionnaires (38%) were returned and analyzed (Table I). Sixty percent of the respondents were in private practice, 40% in academics. Only 11% of the respondents devoted more than 75% of their practice to erectile dysfunction. Forty-one percent had been in practice more than 20 years, and 74% had practiced more than 10 years, indicating an experienced membership in the SSI. The number of prostheses placed per year varied from 10 or less (18%) to greater than 30 (23%). Most (67%) used inflatable prostheses in more than 75% of their patients. AMS devices were favored by 61% and Mentor devices by 39%. The penoscrotal approach was favored by the SSI members (71%), and virtually all respondents placed the reservoirs in a paravesical location. Thirty respondents (29%) had seen reservoir migration, but it was a rare occurrence and was seen almost exclusively in devices placed through a scrotal/penoscrotal incision (97%). A review of the three-piece penile prosthesis procedures used in the practice of one of us (S.K.W.) revealed an incidence of 0.7% (eight migrations in a series of 1206 three-piece penile prostheses). It was unclear whether the herniation was inguinal or high scrotal in location, but it was palpable in all cases. Most incidents happened in the immediate postoperative period and were associated with strong coughing or vomiting, although sporadic reports of patients presenting with herniated reservoirs months after surgery were found. The respondents indicated that these had been “acute” herniations that the patient had initially tolerated and later presented for correction of the defect.
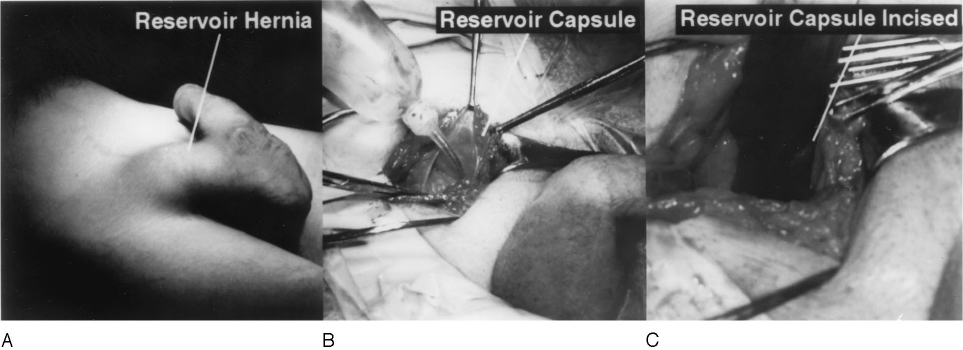
Most surgeons (80%) who were familiar with this complication elected to approach the herniation through an inguinal incision with concomitant closure of the external ring and replacement of the reservoir into its proper location. A few advocated replacement through the same (penoscrotal) incision in patients in whom the herniation was noted in the immediate postoperative period. In cases of a late-presenting hernia, the capsule around the reservoir is mature. This tough, fibrous membrane is incised to allow access to the perivesical space and subsequently used in the closure. If the patient was asymptomatic and had an otherwise functional prosthesis, some surgeons reported having left the reservoir in the inguinal canal or upper scrotum with no ill effects.
COMMENT
Early experience with the inflatable penile prosthesis entailed a high incidence of reoperation for mechanical failure.6,7 With device modification, recent reports show that the revision rate for mechanical failure is quite low. In some series,8,9 revision for human factors (infection, medical problems, physician error, patient dissatisfaction) is considerably higher than for mechanical failure. Recent reports have also demonstrated that the three-piece prostheses manufactured by AMS and Mentor have better mechanical survival than selfcontained10 or two-piece inflatable devices.11 Intravesical and gastrointestinal erosions of reservoirs have been previously reported as isolated, rare incidents.3–5 Since reservoir placement is necessary with the more mechanically dependable three-piece device, we desired to detect the incidence and management of postoperative reservoir herniation. A review of published reports, including those on the safety and efficacy outcomes of inflatable penile prostheses, did not reveal this complication as a specifically encountered entity.12–15
Reservoir herniation is a rare, but consistent, occurrence that may be experienced by surgeons implanting three-piece prostheses. Although the response rate of 38% is not ideal, we do not believe that it skewed the data, as we did not calculate the incidence of herniation based on the questionnaire data. The incidence data was based on the results of one series of 1206 cases of three-piece penile prosthesis surgery.
The results of our survey revealed that reservoir herniation occurs almost exclusively with the scrotal/ penoscrotal approach (97%). Only one respondent reported having seen this complication when an infrapubic incision was used. It would be tempting to suggest the infrapubic incision as a means of avoiding this unusual complication.Webelieve this would be amistake, since the incidence of reservoir herniation is quite low and infrapubic incision carries the possible complication of dorsal nerve injury. 16 The latter complication causes permanent loss of penile sensation and is incurable.
Although our survey did not specifically ask questions regarding the incidence of infection associated with reservoir herniation, none of the respondents made comments concerning infection or managed reservoir herniation by complete device removal, an approach that would have been the likely choice in most cases if infection had been encountered. We did not find prosthesis infection to be associated with intrascrotal/inguinal reservoir herniation in our own series. Our questionnaire design also did not allow an accurate assessment of the incidence of reservoir herniation as a fraction of the total number of prostheses placed by all respondents. However, one of the respondents with a very large series reported a total of eight reservoir migrations of 1206 inflatable prostheses placed (0.7%).
Anecdotal comments from SSI members responding to the survey indicated the major causes of reservoir herniation to be severe postoperative coughing or vomiting, inflation of the prosthesis in the immediate period after implantation, or a preexisting large external inguinal ring. Several more experienced implant surgeons repositioned the reservoir (or replaced it with a larger size) through the same penoscrotal incision if the herniation had occurred acutely. Ring closure was optional. When herniation was discovered long after the original operation, most preferred an inguinal approach, with replacement of the reservoir and closure of the defect (Fig. 1). A few reported asymptomatic patients who had functioning prostheses in the face of acute or chronic reservoir herniation. As long as the patient did not object to the palpable reservoir, these cases were managed successfully without operative intervention.
What can the surgeon do to prevent this complication? When noted by experienced prosthesis surgeons, this complication is nearly always secondary to vigorous coughing and vomiting in the immediate postoperative period. Every effort should be made by the surgical and anesthesia staff to minimize the increased intra-abdominal pressure caused by these events. Suboptimal reservoir positioning may be implicated in cases encountered by less experienced surgeons. In our experience, the initial filling of the reservoir occasionally causes the reservoir to bulge out of the inguinal ring. Although a support stitch may be placed to tighten the ring after reservoir placement, this is not routinely recommended, as it increases the chances of reservoir puncture during the procedure. Reconfirming proper reservoir positioning in the paravesical space at the end of the procedure (before closure of the dartos layer) is always prudent.
CONCLUSIONS
A survey of the SSI members indicated that reservoir herniation after three-piece inflatable penile prosthesis surgery is an unusual complication experienced at least once by nearly 30% of the respondents. This complication occurs almost exclusively in penoscrotally placed prostheses and usually presents in the immediate postoperative period after vigorous coughing or vomiting. Management consists of reservoir replacement through the original incision if acute, and through an inguinal incision with repair of the defect if chronic. Some respondents reported benign neglect with no adverse consequences. Urologists performing three-piece inflatable penile prosthesis surgery should be familiar with this complication and its management.
References
- Lewis RW: Long-term results of penile prosthetic implants. Urol Clin North Am 22: 847–856, 1995.
- Wilson SK, Cleves MA, and Delk JR: Comparison of mechanical reliability of original and enhanced Mentor Alpha 1 penile prosthesis. J Urol 162: 715–718, 1999.
- Singh I, and Godec CJ: Asynchronous erosion of inflatable penile prosthesis into small and large bowel. J Urol 147: 709–710, 1992.
- Luks F, Huntley HN, and Pizzi WF: Small bowel obstruction by an inflatable penile prosthesis reservoir. Surgery 106: 101–104, 1989.
- Nelson RP Jr: Small bowel obstruction secondary to migration of an inflatable penile prosthesis reservoir: recognition and prevention. J Urol 139: 1053–1054, 1988.
- Wilson SK, Wahman GE, and Lange JL: Eleven years’ experience with the inflatable penile prosthesis. J Urol 139: 951–952, 1988.
- Wilson SK, Cleves MA, and Delk JR: Mechanical vs. non-mechanical causes for revision of Mentor Alpha 1 penile prosthesis. Br J Urol 80(suppl 2): 90, 1997.
- Pacik D, Kumstat P, Dolezel J, et al: Implantation of an inflatable penile prosthesis as an effective alternative to surgical treatment for erectile disorders. Rozhl Chir 74: 363–365, 1995.
- Wilson SK, Cleves MA, and Delk JR: Long-term results with Hydroflex and Dynaflex penile prostheses: device survival comparison to multicomponent inflatables. J Urol 155: 1621–1623, 1996.
- George VK, Erkhan S, and Dhabuwala CB: Follow-up with Mentor two-piece inflatable penile prosthesis. Int J Impot Res 7: 17–21, 1995.
- Steinkohl WB, and Leach GE: Mechanical complications associated with Mentor inflatable penile prosthesis. Urology 38: 32–34, 1991.
- Dubocq F, Teffilli MV, Gheiler EL, et al: Long-term mechanical reliability of multicomponent inflatable penile prosthesis: comparison of device survival. Urology 52: 277– 281, 1998.
- Goldstein I, Bertero EB, Kaufman JM, et al: Early experience with the first pre-connected 3-piece inflatable penile prosthesis: the Mentor Alpha-1. J Urol 150: 1814–1818, 1993.
- Govier FE, Gibbons RP, Correa RJ, et al: Mechanical reliability, surgical complications, and patient and partner satisfaction of the modern three-piece inflatable penile prosthesis. Urology 52: 282–286, 1998.
- Goldstein I, Newman L, Baum N, et al: Safety and efficacy outcome of Mentor Alpha-1 inflatable penile prosthesis implantation for impotence treatment. J Urol 157: 833–839, 1997.
- Wilson SK: Pearls, pitfalls and perils of penile prosthesis implantation, in Hellstrom W (Ed): Male Infertility and Sexual Dysfunction. New York, Springer Verlag, 1997.
